This article was written by Gary Finnegan and published by Vaccines Today.
‘Researchers are working on vaccines against cancer, superbugs, and diseases on the rise due to climate change. Many will help adults. But will health systems ‒ and the public ‒ be ready to reap the benefits? ’
Measles, polio, tetanus. Cervical cancer, pertussis, COVID-19. Thousands of vaccine scientists in multiple countries over several decades have achieved a great deal. Together, they have delivered some 35 vaccines that prevent literally millions of deaths every year.
They have eradicated smallpox and driven down rates of vaccine preventable diseases that are now rarely seen in Europe.
However, science is restless by nature. And there are many medical mysteries still to be solved.
The world still needs a HIV vaccine, an RSV vaccine and universal, one-shot protection against all types of flu and COVID-19. Along with vaccines to prevent cancer, therapeutic cancer vaccines seek to turn the body’s immune system against tumour cells, potentially changing forever how we think about vaccination.
There are new threats on the horizon too, catalysed by climate change, our ageing populations, and rising rates of antimicrobial resistance (AMR). These are the challenges that motivate vaccine scientists.
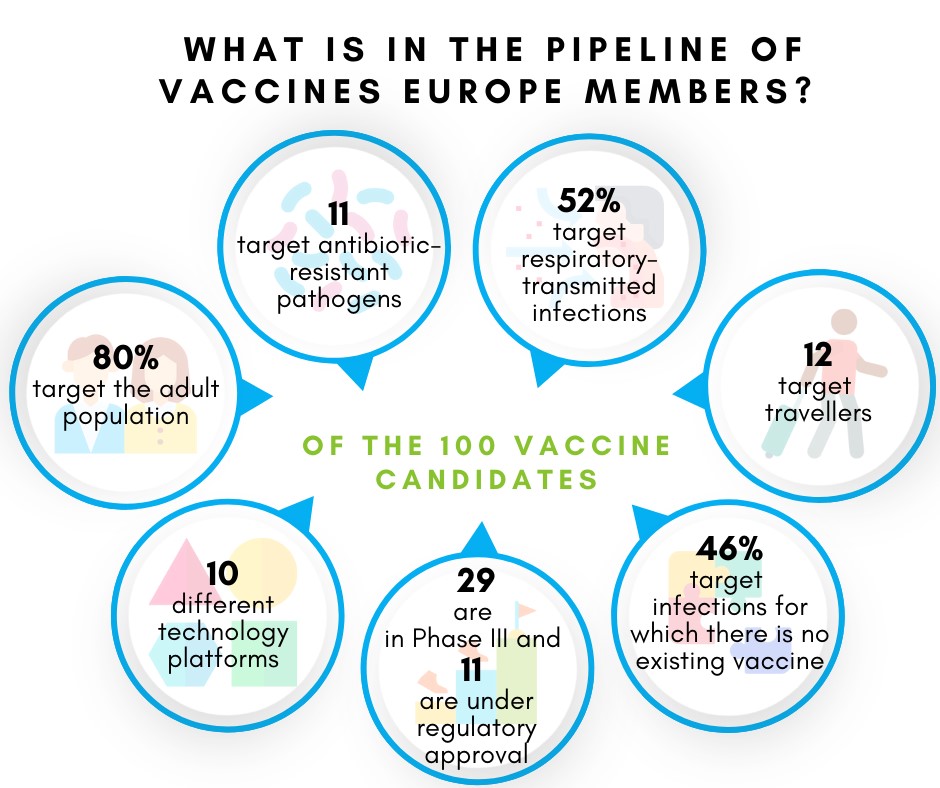
A new review of the research pipeline of Vaccines Europe member companies reveals that there are 100 potential new vaccines at various stages of development. (Vaccines Today is supported by Vaccines Europe.)
Some aim to generate an immune response using traditional methods; others are testing new approaches to protecting against disease. In fact, the 100 vaccines in the pipeline use ten different ‘technology platforms’.
Just over half (54%) of the potential new products are designed to improve on existing vaccines against TB, dengue fever, influenza and COVID-19 ‒ the disease most targeted by vaccine developers. However, demand for new COVID-19 vaccines has declined since the approval of several products two years ago.
The remaining 46% focus on conditions for which there is no vaccine at present: Zika virus, C. difficile (a hospital ‘superbug’), Group B streptococcus, Herpes simplex virus, and others.
AREAS OF GLOBAL UNMET NEED
The 100 vaccines mentioned above include those in development by manufacturers with European links. The full spectrum of products in the pipeline is even larger. For example, the WHO maintains a spreadsheet tracking vaccines in development in areas of high unmet need.
It shows dozens of vaccines in clinical trials against malaria, rotavirus, MERS and lassa fever. Some of the vaccine candidates in this list are included in the Vaccines Europe list, but others are not.
Alongside the efforts of individual companies, partnerships between the public and private sectors aim to expand the impact of vaccination.
For example, the Centre for Epidemic Preparedness Innovations (CEPI) has made ‘Disease X’ a priority for its research grants. Disease X is a placeholder name for a hypothetical new infectious disease with the potential to cause the next pandemic.
This work focused not on the creating a vaccine against any specific disease, but on making sure the vaccine development system is ready to create, test and deliver billions of doses of a new vaccine.
At the same time, the Innovative Health Initiative (IHI), led by the European Commission and the life sciences sector, is running several projects that support the development and uptake of vaccines.
Building demand for immunisation is key to ensuring the use and impact of any new vaccines. Given that 80% of vaccines in development are focused on adults, ensuring uptake among this group is vital.
In late 2022, EU Health Ministers agreed to enhance adult immunisation campaigns and address vaccine hesitancy among people of all ages. Following through on this political commitment is vital: no new vaccine will have any impact unless it is made available to people who need it.
To turn research into reality, adult vaccination must become central to national programmes and the benefits must be communicated to the public. Minimising practical and financial barriers to accessing immunisation is also vital.
In the meantime, researchers will continue to work on vaccines against diseases affecting us today and in the future.